Virtual Meditative Walk
Dr.Diane Gromala, Dr.Chris Shaw, Xin Tong, Servet Ulas, Dr.Owen Williamson, Dr.Pam Squire
Pain experts don’t yet know what causes chronic pain, and so far, there is no cure.
Using VR as the better-known form of ‘pain distraction’ can be helpful for short-term “breakthrough” pain,
but it doesn’t last after you take the VR gear off.
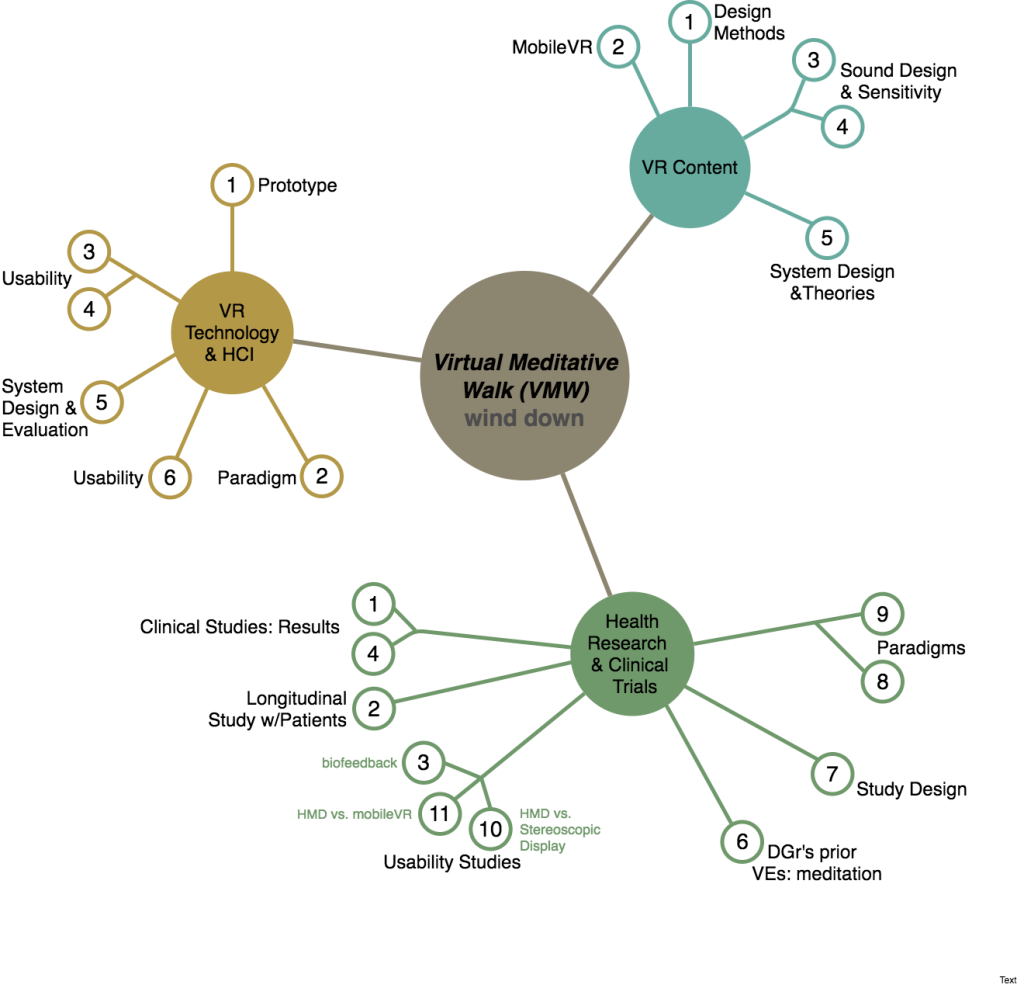
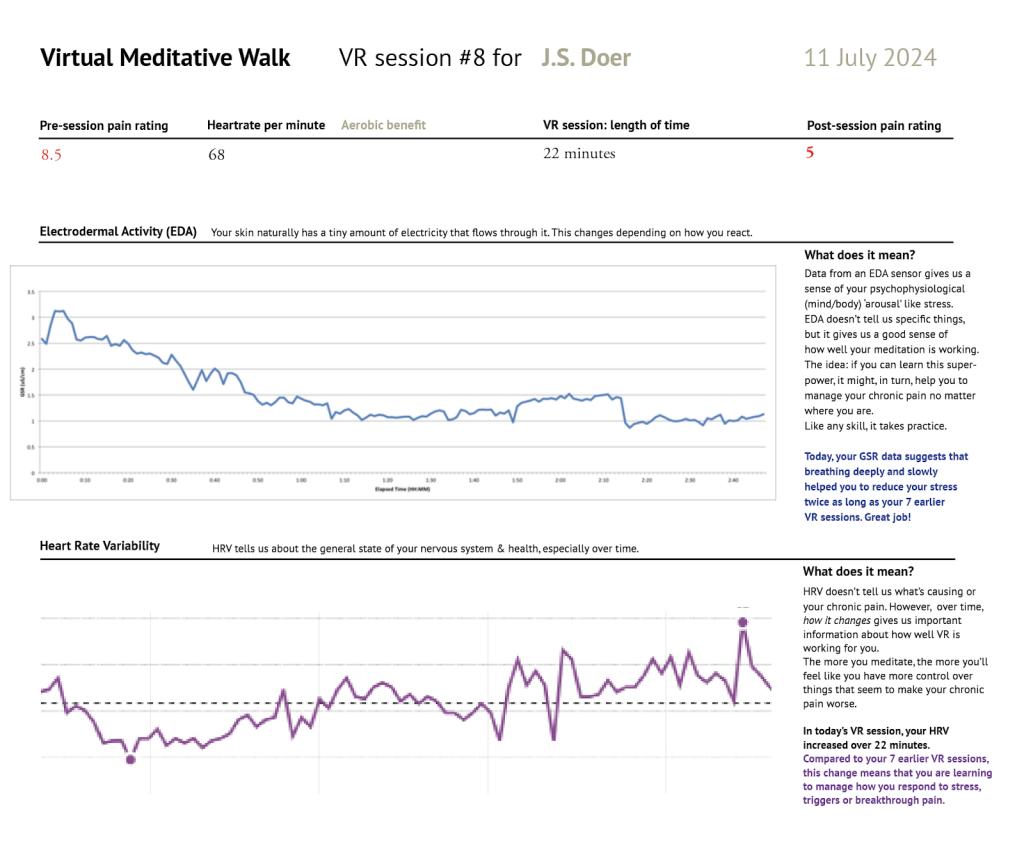
We wonder: if people use VR to build new neural pathways, might those pathways escape the dysfunctional way chronic pain is processed? While we explore that, we are updating our VR interventions for people who live with persistent pain. Our virtual environments are made to calm a usually overactive neurological system, to help patients become or maintain physical activity, and to confront the social stigma that they face. Currently, via a central dashboard, we’re updating the way we visualize self-reported pain data over time and alert users to what seems to be affecting their pain (potential causes and effects), how well users learn to calm their states, and identify what triggers their pain and to see if tracking one’s function & quality of life can matter.

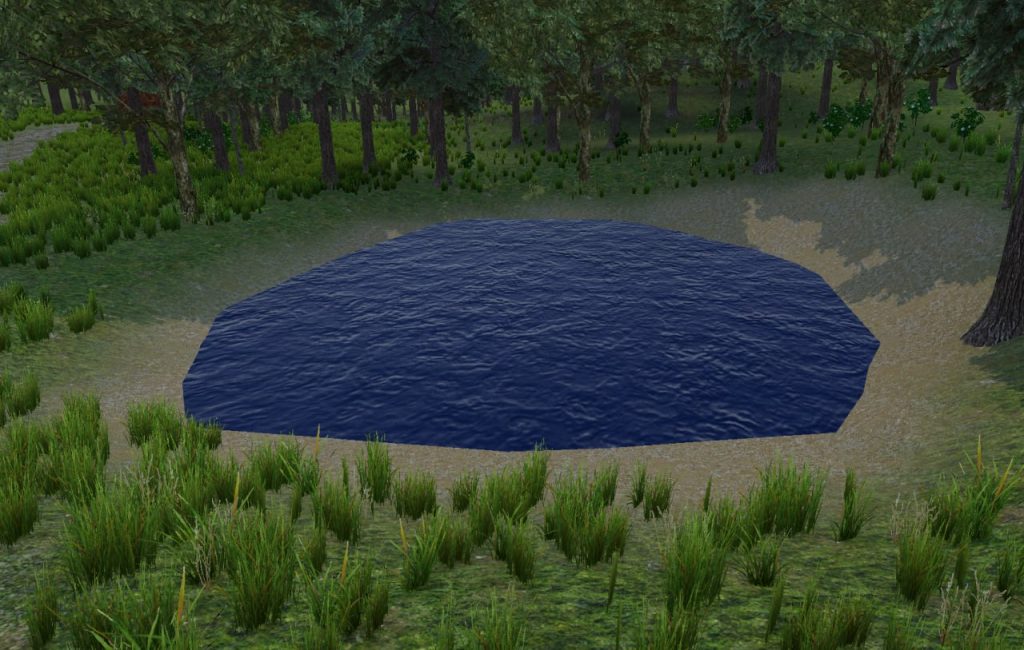 Fig.1 An image of the pond in the Virtual Meditative Walk
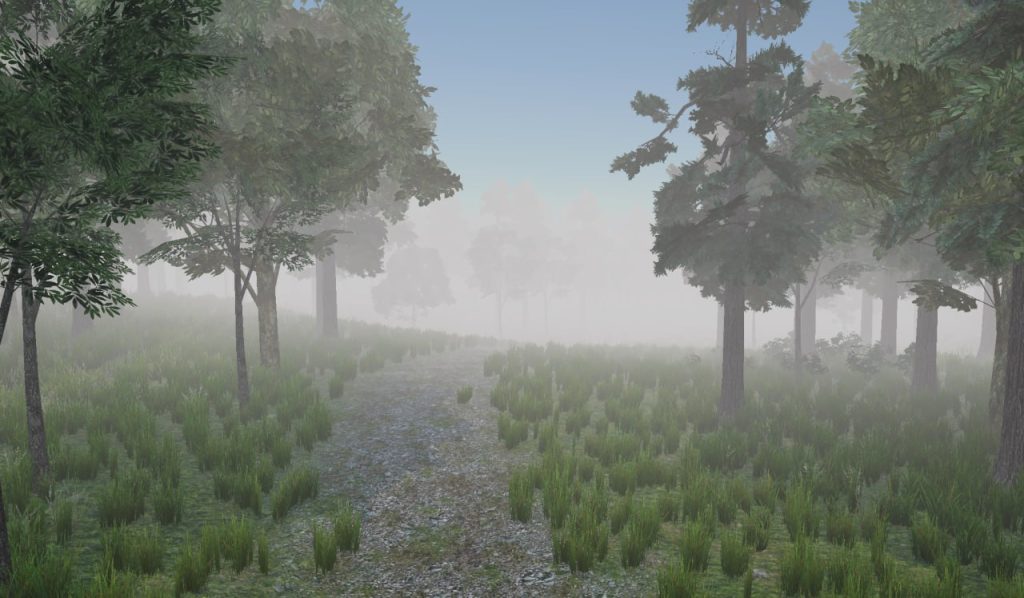
Fig.1 An image of the pond in the Virtual Meditative Walk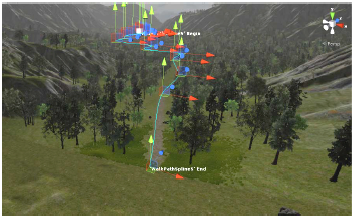 Fig.2 Virtual Meditative Walk:
Fig.2 Virtual Meditative Walk: